Conteúdo
What is the 3-3-3 rule colic?
“`html
Infantile colic can be distressing to parents whose infant is inconsolable during crying episodes. Colic is often defined by the “rule of three”: crying for more than three hours per day, for more than three days per week, and for longer than three weeks in an infant who is well-fed and otherwise healthy. The physician’s role is to ensure that there is no organic cause for the crying, offer balanced advice on treatments, and provide support to the family.
Colic is a diagnosis of exclusion that is made after performing a careful history and physical examination to rule out less common organic causes. Treatment is limited. Feeding changes usually are not advised. Medications available in the United States have not been proved effective in the treatment of colic, and most behavior interventions have not been proved to be more effective than placebo. Families may turn to untested resources for help, and the physician should offer sound advice about these treatments. Above all, parents need reassurance that their baby is healthy and that colic is self-limited with no long-term adverse effects.
Physicians should watch for signs of continuing distress in the child and family, particularly in families whose resources are strained already. Excessive crying or colic in an infant during the first few months of life can be alarming for physicians and parents. Estimates of the occurrence of infantile colic in community-based samples vary from 5 to 25 percent of infants, depending on study design, definition of colic, and method of data collection.
Fussing and crying are normal aspects of development during the first three months of life. During this time, infants cry an average of 2.2 hours per day, peaking at six weeks of age and gradually decreasing. Parents who think their infant cries excessively may seek a physician’s help. Physicians and parents use the term colic to describe an infant with excessive crying, irritability, or fussiness.
The most commonly accepted definition of colic, which originated in 1954, describes using the “rule of three”: crying for more than three hours per day, for more than three days per week, and for more than three weeks in an infant that is well-fed and otherwise healthy. This definition has been used repeatedly in clinical studies of colic.
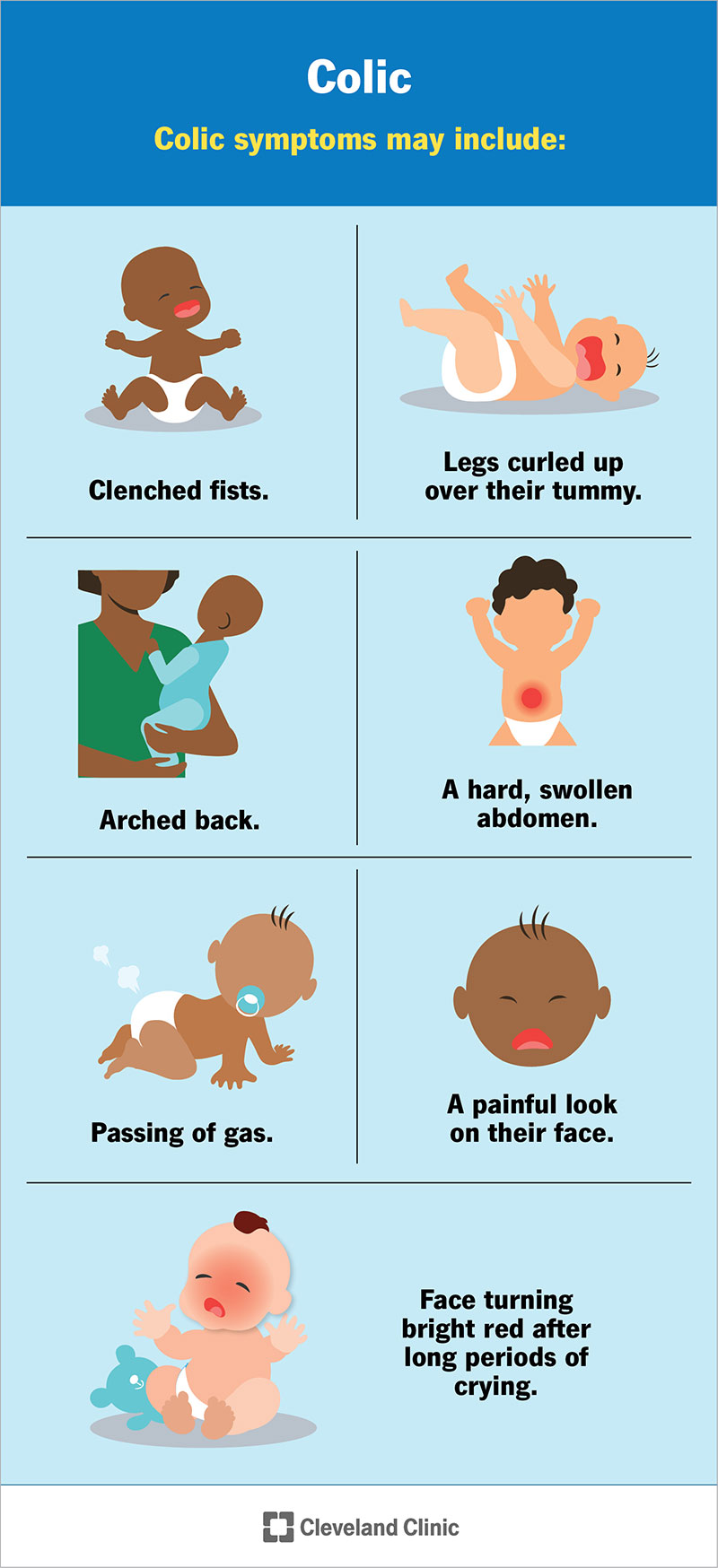
The motor behaviors of infants with colic also were first described in 1954. Colicky infants have attacks of screaming in the evening with associated motor behaviors such as flushed face, furrowed brow, and clenched fists. The legs are pulled up to the abdomen, and the infants emit a piercing, high-pitched scream. Behavior characteristics usually are classified by the timing of the event, paroxysmal crying, and associated behaviors.
Colic typically begins at two weeks of age and usually resolves by four months of age. Crying is concentrated in the late afternoon and evening, occurs in prolonged bouts, and is unpredictable and spontaneous. It appears to be unrelated to environment.
“`
What are the worst weeks for colic?
“`html
If your baby cries for longer than 3 hours a day, your baby might have colic. Colic is not caused by another medical problem. Many babies go through a fussy period. Some cry more than others. If you have a baby with colic, you are not alone. One in five babies cry enough that people call them colicky. Colic usually starts when babies are about 3 weeks old. It gets worse when they are between 4 and 6 weeks old. Most of the time, colicky babies get better after they are 6 weeks old, and are completely fine by the time they are 12 weeks old.
Colic normally begins at about the same time every day. Babies with colic are usually fussier in the evenings. Colic symptoms often begin suddenly. Your baby’s hands may be in a fist. The legs may curl up and the belly may seem swollen. Crying may last for minutes to hours. Crying often calms down when your baby is tired or when gas or stool is passed.
Even though colicky babies look like they have belly pain, they eat well and gain weight normally. Causes of colic may include any of the following:
- People around your baby may also seem worried, anxious, or depressed.
- Often the exact cause of colic is unknown.
Your baby’s health care provider can often diagnose colic by asking you about the baby’s medical history, symptoms, and how long the crying lasts. Your baby’s provider will perform a physical exam and may do some tests to check your baby. Your baby’s provider needs to make sure your baby does not have other medical problems, such as reflux, a hernia, or intussusception.
Foods that are passed through your breast milk to your baby may trigger colic. If your baby is colicky and you are breastfeeding, avoid eating or drinking the following foods for a few weeks to see if that helps. Some breastfeeding moms avoid eating broccoli, cabbage, beans, and other gas-producing foods. But research has not shown that these foods can have a negative effect on your baby. Other possible triggers include:
Talk to a lactation consultant to learn more about the possible causes related to breastfeeding.
What comforts one baby may not calm another. And what calms your baby during one episode may not work for the next. But try different techniques and revisit what seems to help, even if it only helps a little.
If you breastfeed: Sometimes it can be really hard to stop your baby from crying. Here are techniques you may want to try:
Your baby will most likely outgrow colic by 3 to 4 months of age. There are usually no complications from colic. Parents can get really stressed when a baby cries a lot. Know when you have reached your limit and ask family members or friends to help. If you feel like you may shake or hurt your baby, get help right away.
Call your baby’s provider if your baby is:
You need to make sure that your baby does not have any serious medical problems. Call your baby’s provider right away if:
Get help right away for yourself if you feel overwhelmed or have thoughts of harming your baby.
Infantile colic – self-care; Fussy baby – colic
“`
How do you get rid of colic in babies fast?
“`html
Your baby’s care provider will do a complete physical exam to identify any possible causes for your baby’s distress. The exam will include:
- Lab tests
- X-rays
- Other diagnostic tests
Lab tests, X-rays and other diagnostic tests aren’t usually needed, but in unclear cases they help to exclude other conditions as possible causes. The primary goals are to soothe the child as much as possible with a variety of interventions and ensure that parents have the support they need to cope.
You may find it helpful to have a plan, a list of soothing strategies you can try. You may need to experiment. Some may work better than others, and some may work one time but not another. Soothing strategies may include:
- Changes in feeding practices may also provide some relief. Bottle-feed your baby in an upright position and burp frequently during and after a feeding.
- Using a curved bottle will help with upright feeding, and a collapsible bag bottle can reduce the intake of air.
If soothing or feeding practices aren’t reducing crying or irritability, your doctor may recommend a short-term trial of dietary changes. If your baby has a food allergy, however, there would likely be other signs and symptoms, such as a rash, wheezing, vomiting or diarrhea. Dietary changes may include:
Caring for an infant who has colic can be exhausting and stressful, even for experienced parents. The following strategies can help you take care of yourself and get the support you need:
One factor that may contribute to colic is an imbalance of the helpful bacteria in an infant’s digestive tract. One treatment under investigation is the use of good bacteria (probiotics) to create an appropriate bacterial balance to improve overall digestive health.
Some studies have shown a reduction in crying times when babies with colic were treated with a bacterium called Lactobacillus reuteri. The studies have been conducted with small groups, and results have been somewhat mixed. Most experts agree there’s not enough evidence at this time to support the use of probiotics to treat colic.
Several small studies have shown some benefits or mixed results for alternative treatments. There’s not enough evidence, however, to judge the potential benefit over the risks. Alternative remedies under investigation include:
Known risks include the following issues:
Talk to your baby’s care provider before using an alternative medicine to treat your infant for colic.
It’s a good idea to prepare ahead of time for an appointment with your baby’s health care provider. Here’s some information to help you get ready.
To prepare for your appointment, make some notes about:
- Write down any additional questions you have about your baby’s health or development.
During your appointment, don’t hesitate to ask any other questions as they occur to you. Your baby’s care provider is likely to ask a number of questions, such as:
- Your answers to these questions can help your baby’s care provider determine if there are other conditions that may be contributing to crying and discomfort.
Your Annual F
“`
At what age does colic pain end in babies?
“`html
Colic is frequent, prolonged and intense crying or fussiness in a healthy infant. Colic can be particularly frustrating for parents because the baby’s distress occurs for no apparent reason and no amount of consoling seems to bring any relief. These episodes often occur in the evening, when parents themselves are often tired.
Episodes of colic usually peak when an infant is about 6 weeks old and decline significantly after 3 to 4 months of age. While the excessive crying will resolve with time, managing colic adds significant stress to caring for your newborn child. You can take steps that may lessen the severity and duration of colic episodes, alleviate your own stress, and bolster confidence in your parent-child connection.
Babies have been known to fuss and cry, especially during the first three months of life. The range for what’s considered typical crying is difficult to pin down. In general, colic is defined as crying for three or more hours a day, three or more days a week, for three or more weeks.
Features of colic may include the following:
- Sometimes there is relief in symptoms after the infant passes gas or has a bowel movement. Gas is likely the result of swallowed air during prolonged crying.
- Excessive, inconsolable crying may be colic or an indication of an illness or condition that causes pain or discomfort. Schedule an appointment with your child’s health care provider for a thorough exam if your infant experiences excessive crying or other signs or symptoms of colic.
The cause of colic is unknown. It may result from numerous contributing factors. While a number of causes have been explored, it’s difficult for researchers to account for all the important features, such as why it usually begins late in the first month of life, how it varies among infants, why it happens at certain times of day and why it resolves on its own in time.
Possible contributing factors that have been explored include:
- Risk factors for colic are not well-understood. Research has not shown differences in risk when the following factors were considered:
- Infants born to mothers who smoked during pregnancy or after delivery have an increased risk of developing colic.
Colic does not cause short-term or long-term medical problems for a child. Colic is stressful for parents. Research has shown an association between colic and the following problems with parent well-being:
The stress of calming a crying baby has sometimes prompted parents to shake or otherwise harm their child. Shaking a baby can cause serious damage to the brain and death. The risk of these uncontrolled reactions is greater if parents don’t have information about soothing a crying child, education about colic and the support needed for caring for an infant with colic.
Your Annual Fund gift can drive advancements in cancer care.
“`
How do you relieve colic pain in babies?
“`html
Your baby’s care provider will do a complete physical exam to identify any possible causes for your baby’s distress. The exam will include:
Lab tests, X-rays and other diagnostic tests aren’t usually needed, but in unclear cases they help to exclude other conditions as possible causes. The primary goals are to soothe the child as much as possible with a variety of interventions and ensure that parents have the support they need to cope.
You may find it helpful to have a plan, a list of soothing strategies you can try. You may need to experiment. Some may work better than others, and some may work one time but not another. Soothing strategies may include:
- Changes in feeding practices may also provide some relief. Bottle-feed your baby in an upright position and burp frequently during and after a feeding.
- Using a curved bottle will help with upright feeding, and a collapsible bag bottle can reduce the intake of air.
If soothing or feeding practices aren’t reducing crying or irritability, your doctor may recommend a short-term trial of dietary changes. If your baby has a food allergy, however, there would likely be other signs and symptoms, such as a rash, wheezing, vomiting or diarrhea. Dietary changes may include:
Caring for an infant who has colic can be exhausting and stressful, even for experienced parents. The following strategies can help you take care of yourself and get the support you need:
One factor that may contribute to colic is an imbalance of the helpful bacteria in an infant’s digestive tract. One treatment under investigation is the use of good bacteria (probiotics) to create an appropriate bacterial balance to improve overall digestive health.
Some studies have shown a reduction in crying times when babies with colic were treated with a bacterium called Lactobacillus reuteri. The studies have been conducted with small groups, and results have been somewhat mixed. Most experts agree there’s not enough evidence at this time to support the use of probiotics to treat colic.
Several small studies have shown some benefits or mixed results for alternative treatments. There’s not enough evidence, however, to judge the potential benefit over the risks. Alternative remedies under investigation include:
Known risks include the following issues:
Talk to your baby’s care provider before using an alternative medicine to treat your infant for colic.
It’s a good idea to prepare ahead of time for an appointment with your baby’s health care provider. Here’s some information to help you get ready.
To prepare for your appointment, make some notes about:
- Write down any additional questions you have about your baby’s health or development.
During your appointment, don’t hesitate to ask any other questions as they occur to you. Your baby’s care provider is likely to ask a number of questions, such as:
Your answers to these questions can help your baby’s care provider determine if there are other conditions that may be contributing to crying and discomfort.
Your Annual F
“`
What is the 3 3 3 rule for colic?
“`html
Infantile colic can be distressing to parents whose infant is inconsolable during crying episodes. Colic is often defined by the “rule of three”: crying for more than three hours per day, for more than three days per week, and for longer than three weeks in an infant who is well-fed and otherwise healthy. The physician’s role is to ensure that there is no organic cause for the crying, offer balanced advice on treatments, and provide support to the family. Colic is a diagnosis of exclusion that is made after performing a careful history and physical examination to rule out less common organic causes.
Treatment is limited. Feeding changes usually are not advised. Medications available in the United States have not been proved effective in the treatment of colic, and most behavior interventions have not been proved to be more effective than placebo. Families may turn to untested resources for help, and the physician should offer sound advice about these treatments. Above all, parents need reassurance that their baby is healthy and that colic is self-limited with no long-term adverse effects. Physicians should watch for signs of continuing distress in the child and family, particularly in families whose resources are strained already.
Excessive crying or colic in an infant during the first few months of life can be alarming for physicians and parents. Estimates of the occurrence of infantile colic in community-based samples vary from 5 to 25 percent of infants, depending on study design, definition of colic, and method of data collection.
Fussing and crying are normal aspects of development during the first three months of life. During this time, infants cry an average of 2.2 hours per day, peaking at six weeks of age and gradually decreasing. Parents who think their infant cries excessively may seek a physician’s help.
Physicians and parents use the term colic to describe an infant with excessive crying, irritability, or fussiness. The most commonly accepted definition of colic, which originated in 1954, describes using the “rule of three”: crying for more than three hours per day, for more than three days per week, and for more than three weeks in an infant that is well-fed and otherwise healthy. This definition has been used repeatedly in clinical studies of colic. The motor behaviors of infants with colic also were first described in 1954.
Colicky infants have attacks of screaming in the evening with associated motor behaviors such as flushed face, furrowed brow, and clenched fists. The legs are pulled up to the abdomen, and the infants emit a piercing, high-pitched scream.
Behavior characteristics usually are classified by the timing of the event, paroxysmal crying, and associated behaviors. Colic typically begins at two weeks of age and usually resolves by four months of age. Crying is concentrated in the late afternoon and evening, occurs in prolonged bouts, and is unpredictable and spontaneous. It appears to be unrelated to the environment.
“`
What worsens colic?
“`html
If your baby cries for longer than 3 hours a day, your baby might have colic. Colic is not caused by another medical problem. Many babies go through a fussy period. Some cry more than others.
If you have a baby with colic, you are not alone. One in five babies cry enough that people call them colicky. Colic usually starts when babies are about 3 weeks old. It gets worse when they are between 4 and 6 weeks old. Most of the time, colicky babies get better after they are 6 weeks old, and are completely fine by the time they are 12 weeks old.
Colic normally begins at about the same time every day. Babies with colic are usually fussier in the evenings. Colic symptoms often begin suddenly. Your baby’s hands may be in a fist. The legs may curl up and the belly may seem swollen. Crying may last for minutes to hours. Crying often calms down when your baby is tired or when gas or stool is passed.
Even though colicky babies look like they have belly pain, they eat well and gain weight normally.
Causes of colic may include any of the following:
- People around your baby may also seem worried, anxious, or depressed.
Often the exact cause of colic is unknown. Your baby’s health care provider can often diagnose colic by asking you about the baby’s medical history, symptoms, and how long the crying lasts. Your baby’s provider will perform a physical exam and may do some tests to check your baby. Your baby’s provider needs to make sure your baby does not have other medical problems, such as reflux, a hernia, or intussusception. Foods that are passed through your breast milk to your baby may trigger colic. If your baby is colicky and you are breastfeeding, avoid eating or drinking the following foods for a few weeks to see if that helps.
Some breastfeeding moms avoid eating broccoli, cabbage, beans, and other gas-producing foods. But research has not shown that these foods can have a negative effect on your baby. Other possible triggers include:
- Talk to a lactation consultant to learn more about the possible causes related to breastfeeding.
What comforts one baby may not calm another. And what calms your baby during one episode may not work for the next. But try different techniques and revisit what seems to help, even if it only helps a little.
If you breastfeed: Sometimes it can be really hard to stop your baby from crying. Here are techniques you may want to try:
Your baby will most likely outgrow colic by 3 to 4 months of age. There are usually no complications from colic. Parents can get really stressed when a baby cries a lot. Know when you have reached your limit and ask family members or friends to help. If you feel like you may shake or hurt your baby, get help right away.
Call your baby’s provider if your baby is:
- You need to make sure that your baby does not have any serious medical problems.
Call your baby’s provider right away if:
Get help right away for yourself if you feel overwhelmed or have thoughts of harming your baby.
Infantile colic – self-care; Fussy baby – colic
“`
Is it okay to let colic babies cry?
“`html
Baby’s Got Colic and You Can’t Cope
As new parents will attest, there’s almost nothing more unnerving than a crying baby. Worse still? An infant who won’t stop crying, regardless of what you do. If your baby fits this bill, it could signify that dreaded C-word: colic.
As many as one in five infants are colicky, a condition characterized by inconsolable crying and fretfulness for hours at a time — sometimes round-the-clock but usually at the same time of day, typically in the late afternoon or evening. These babies often have excessive gas and may repeatedly pull their knees to their stomachs and clench their fists in distress.
The causes of colic still largely remain a mystery, although the most common theories are that colicky kids either have an immature digestive tract or nervous system, or that their temperaments make them prone to overstimulation or less adept at self-quieting. Nor is there a definitive test or X-ray doctors can use to diagnose colic in infants.
“Colic is a diagnosis of exclusion, which means you don’t have another good explanation for it,” says Dr. Terry Hatch, associate professor of pediatrics at University of Illinois College of Medicine in Champaign-Urbana.
A boa notícia é que, se for apenas cólica — que geralmente aparece entre 2 semanas e 4 semanas de idade — seu bebê não está em perigo físico, e o remédio é relativamente simples: esperar. Felizmente, não há evidências de que a cólica seja um sinal de doença crônica a caminho ou que ter um bebê com cólica aumente seu risco de ter outro.
“Colic is usually associated with a normal, healthy growing child,” says Dr. Rob Squires, associate professor of pediatrics at University of Texas Southwestern Medical Center in Dallas and chair of the American Academy of Pediatrics’ section on gastroenterology and nutrition.
Colic typically disappears by age 3 months or 4 months, but unfortunately, there’s no tried-and-true remedy for the problem. Doctors say that while certain measures may offer some relief some of the time, a sudden, miraculous cure probably means your baby was ready to outgrow the condition on their own anyway.
But the lack of a proven cure doesn’t mean parents should ignore a baby’s distress, either. For starters, if crying persists after you make the obvious checks — dirty diaper? hungry? — check with your doctor, who’ll want to rule out any underlying medical conditions, such as allergies or gastroesophageal reflux (similar to adult heartburn).
Keep a log detailing your baby’s fussy periods to help determine what, if anything, seems to trigger or relieve the discomfort. If you’re a nursing mom, your doctor may suggest cutting dairy or gas-producing foods from your diet. Milk and soy formulas also may upset infant tummies, in which case a predigested hypoallergenic type formula may help.
If the verdict is colic, try to keep your cool — even if the only way you can do that is by silently walking the halls with your screaming baby fastened securely in a Snugli infant carrier.
“`